Scientific Resources
Key points from PRIMARY Scoring publications
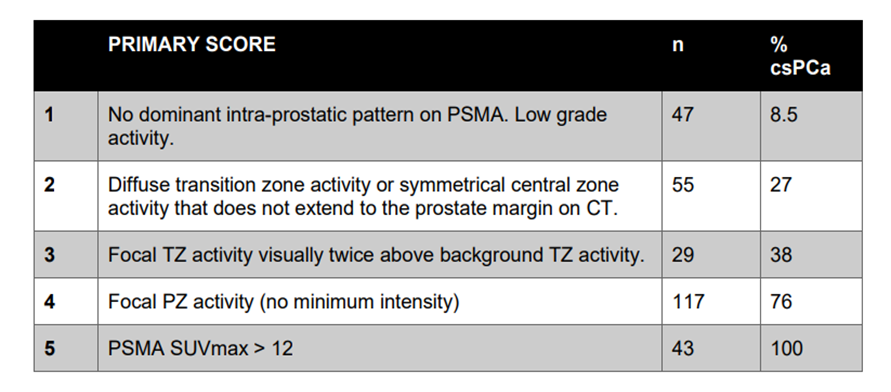
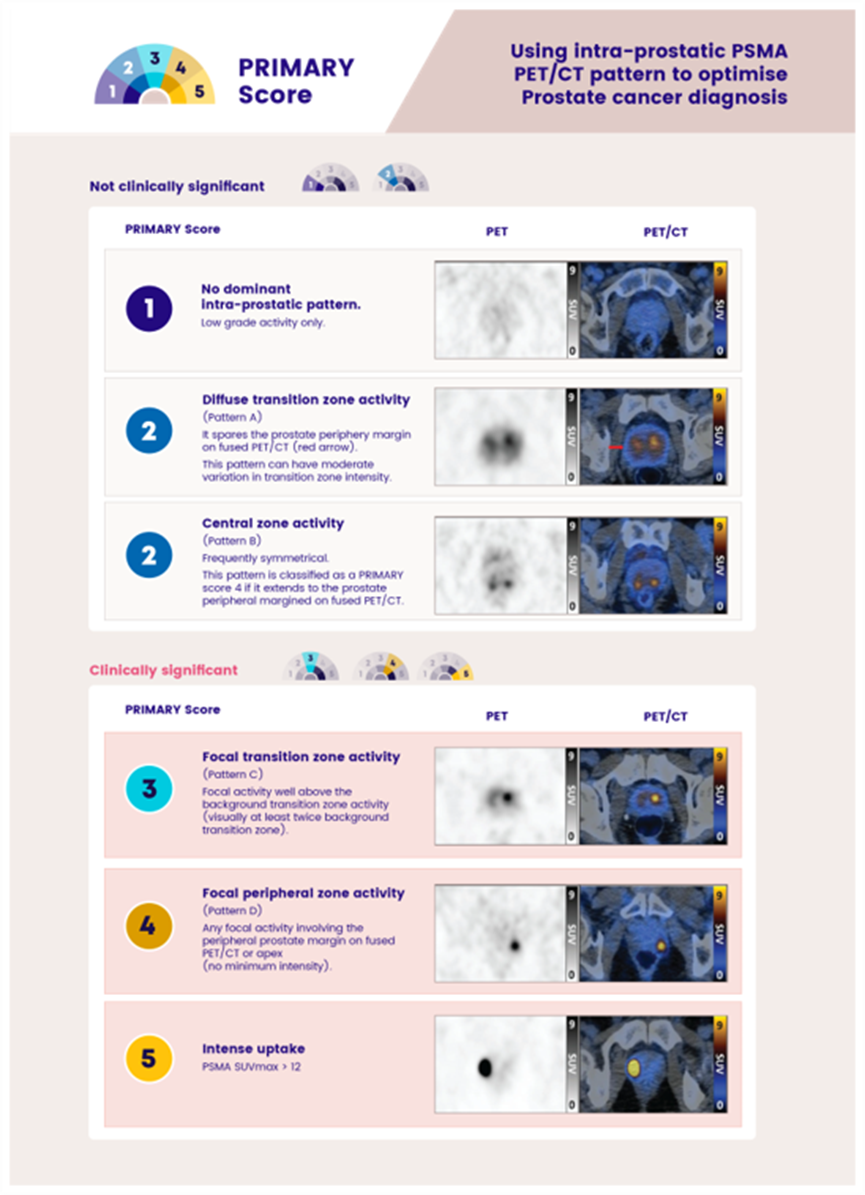
The PRIMARY score is a 5-category scale developed to identify clinically significant intraprostate malignancy (csPCa) on 68Ga-prostatespecific membrane antigen (PSMA) PET/CT (68Ga-PSMA PET) using a combination of anatomic site, pattern, and intensity.
This scoring system incorporating intraprostatic patterns and intensity on 68Ga-PSMA PET/CT shows potential as an accurate method for diagnosing csPCa and should be considered when PSMA PET is undertaken for this purpose.
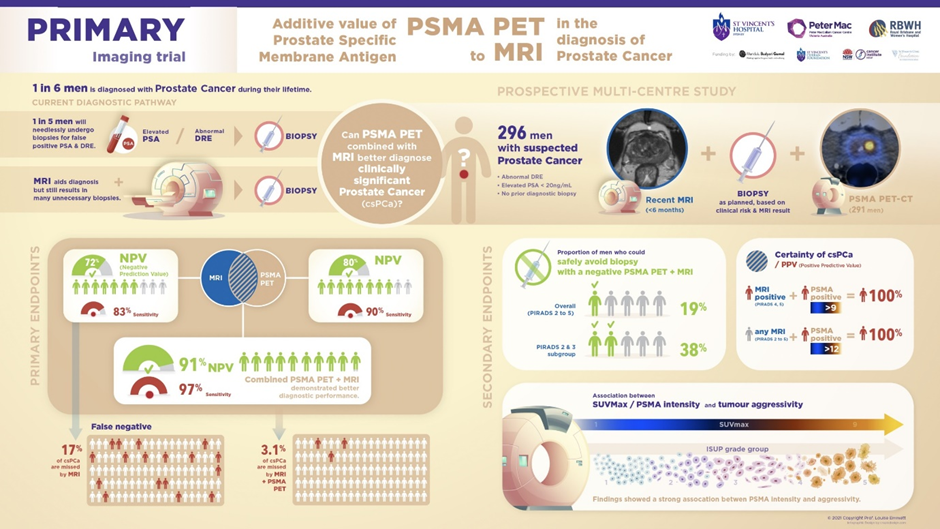
Multiparametric MRI (mpMRI) is currently the standard of care for the diagnosis of prostate cancer, with validated standardization of reporting using the Prostate Imaging Reporting and Data System (PI-RADS). However, if clinically significant prostate cancer (sPCa) was defined as GG _2, approximately 25% of men with negative mpMRI findings had malignancy that was missed.
Prostate-specific membrane antigen (PSMA) is a large transmembrane glycoprotein that is highly overexpressed in prostate adenocarcinoma. 68Ga-PSMA-11 PET/CT (68Ga-PSMA PET/CT) has recently been reported to demonstrate similar diagnostic accuracy to MRI for the diagnosis of prostate cancer, with significant improvement in negative predictive value if the 2 modalities are used in combination.
PSMA activity in intraprostatic processes such as benign prostatic hypertrophy, prostate intraepithelial neoplasia, and low-grade International Society of Urological Pathology (ISUP) grade group 1 malignancy can be difficult to distinguish from csPCa on the basis of PSMA intensity alone.
5-level PRIMARY score incorporating intraprostatic pattern and intensity on 68Ga-PSMA PET/CT shows potential for diagnosing csPCa with high accuracy.
The recent studies confirmed that the use of pattern and intensity within a 5-level score (PRIMARY) is reproducible between readers, with an increased or equivalent diagnostic accuracy for the detection of csPCa compared with mpMRI.
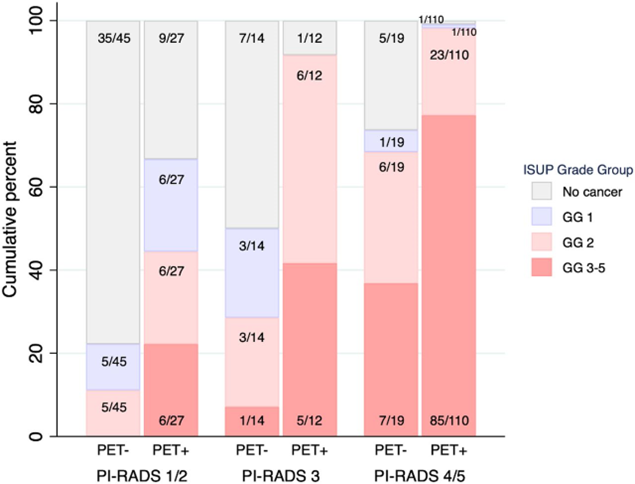
PRIMARY found a significant improvement in both negative predictive value (NPV) (91%, 95% confidence interval [CI] 80–97% vs 72%, 95% CI 61–80%; p < 0.001) and sensitivity (97%, 95% CI 93–99% vs 83%, 95% CI 77–89%; p < 0.001) for PSMA PET/CT in addition to mpMRI versus mpMRI alone. The most significant additional value of PSMA PET/CT was for participants with high clinical risk and PI-RADS 2 or 3 lesions.
According to the results from the PRIMARY trial, PSMA PET/CT and mpMRI appear to be a powerful combination for identification of significant malignancy, particularly for PIRADS 2 or 3 lesions with high clinical risk, that could potentially increase the detection of sPCa and reduce both the number of biopsies undertaken and the diagnosis of insignificant malignancy requiring additional follow-up. An imaging examination is considered negative for PRIMARY scores 1–2 versus positive for PRIMARY scores 3–5.
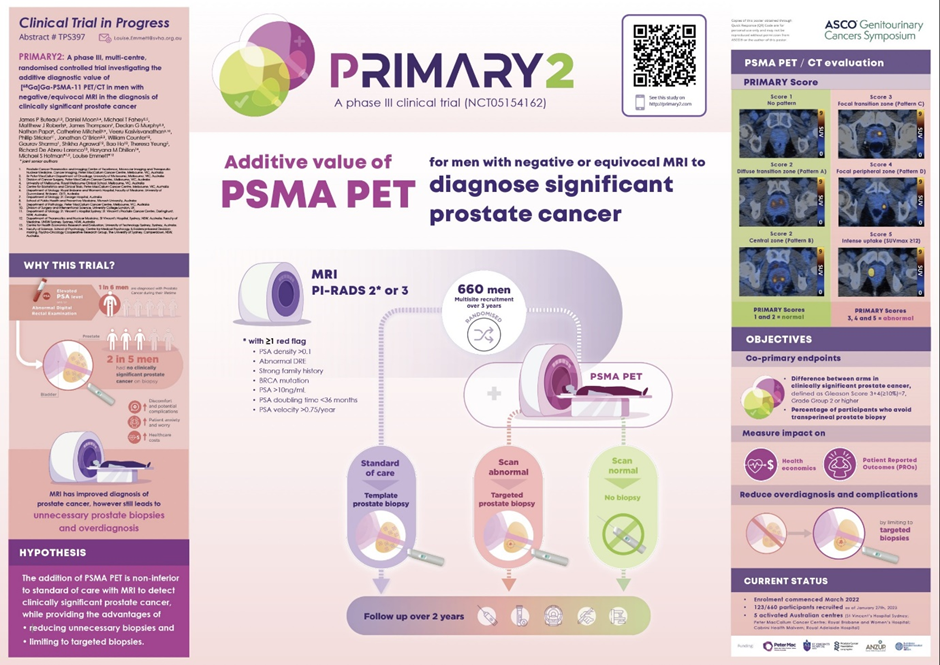
The PSMA PET/CT intervention is found to be noninferior, the diagnostic pathway for diagnosis of sPCa will be enhanced by avoiding unnecessary prostate biopsies. Furthermore, PSMA PET/CT guidance for transperineal prostate biopsy could both improve targeting, by identifying sites suspicious for sPCa, and reduce overdiagnosis of GG 1 disease that may be identified on template transperineal prostate biopsy. These approaches could reduce patient anxiety and worry about having prostate cancer, and decrease biopsy complications via better triaging and targeted biopsies.
The PRIMARY score was developed to optimize the diagnostic accuracy of 68Ga-PSMA PET for csPCa intraprostatically and particularly to improve specificity over an SUVmax-based reporting method. The PRIMARY score has been incorporated into PROMISE version 2 for reporting of 68Ga-PSMA PET.
The validation study undertaken on a real-world dataset confirmed the high diagnostic accuracy of the PRIMARY score, with significant reproducibility among readers. Accuracy was equivalent to the MRI PI-RADS score, with better reproducibility, despite the limited experience of the readers with the PRIMARY score.
Benign intraprostatic patterns of PSMA activity with increased uptake in the transition and central zones are common as a result of benign prostatic hypertrophy and physiologic activity surrounding the ejaculatory ducts in the central zones. However, most malignancy (70%) arises within the peripheral zone of the prostate, with the incidence of transition and central zone malignancy significantly lower. The PRIMARY score uses this information to weight focal activity in the peripheral and transition zones while classifying diffuse transition zone activity as a benign finding.
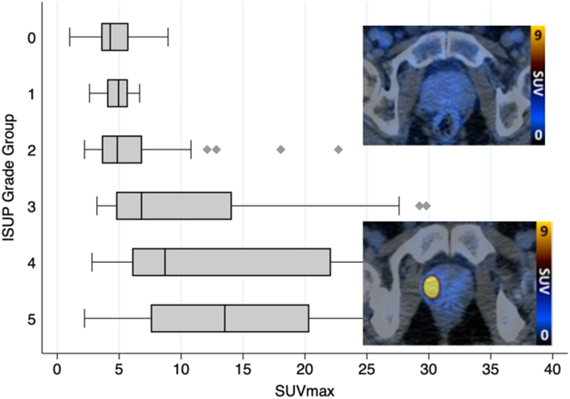
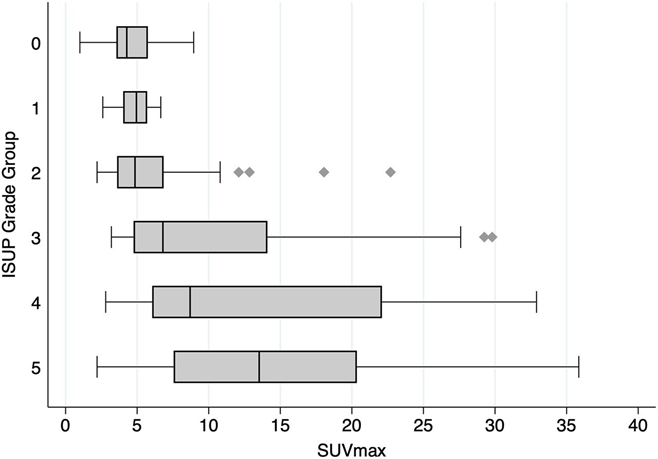
The initial PRIMARY score publication found that separating patterns of intraprostatic PSMA activity into focal or diffuse improved identification of significant malignancy. This validation cohort confirmed improved specificity using a pattern-based reporting system rather than an intensity (SUVmax)-based analysis as was used in the initial PRIMARY paper.
68Ga-PSMA PET using the PRIMARY score in conjunction with mpMRI may further optimize the diagnosis of prostate cancer, reducing the biopsy requirement and detection of insignificant malignancy while improving sensitivity for csPCa.
This is being evaluated further in the prospective randomized PRIMARY2 trial (NCT05154162).
There is a strong association between ISUP grade group on histopathology and 68Ga-PSMA PET intensity, an association that is likely due to the pro-proliferative role of the PSMA receptor in prostate cancer. As with the PRIMARY study, the analysis found that an SUVmax of more than 12 was associated with csPCa in 100%, with an ISUP grade group of at least 3 in 93% of those cases. This finding validates the use of PSMA intensity (SUVmax 12) as the maximal PRIMARY score, although further work will be required to identify an optimum intensity for a PRIMARY score of 5 if PSMA-targeting peptides other than 68Ga-PSMA are to be utilized.
The PRIMARY score showed substantial interrater reproducibility by first-user nuclear medicine specialists, exceeding that of PI-RADS. Diagnostic performance was similar between the 2 modalities. The PRIMARY score should be considered when interpreting intraprostatic PSMA PET images.
The PRIMARY score is equivalent in diagnostic accuracy to mpMRI when undertaken prior to prostate biopsy in a high-risk population. Further, it is more reproducible than mpMRI despite the readers having limited clinical experience with the score.
A 5-level PRIMARY score incorporating intraprostatic patterns and intensity on 68Ga-PSMA PET/CT shows potential as an accurate method for diagnosing csPCa and should be considered when PSMA PET is undertaken for this purpose.
PRIMARY II, the first prospective multicentre trial to evaluate the potential of PSMA PET (PSMA) for the diagnosis of intraprostatic malignancy in men with MRI PI-RADS 2–5, found that the combination of PSMA + MRI improved sensitivity and NPV for csPCa compared with MRI alone, while identifying a further proportion of men who could safely avoid biopsy over and above an MRI triaged approach.
PSMA + MRI improved NPV and sensitivity for csPCa in an MRI triaged population. Further randomised studies will determine whether biopsy can safely be omitted in men with a high clinical suspicion of csPCa but negative combined imaging.
PRIMARY Score Definition
PRIMARY & PRIMARY 2 schemas:
PRIMARY Publications: